Mouth ulcers are sores that develop on the soft tissues inside the mouth. Many are harmless and temporary. Some can signal infection, immune disorders, nutritional deficiencies, systemic inflammatory disease, or (rarely) oral cancer.
This guide focuses on what you can often recognize at home: color, shape, location, texture, pain, timing, and the red flags that should push you to get checked.
Important (Medical disclaimer)
This is general information. If you are unsure what you are seeing, or if a sore is not healing, get evaluated by a clinician or dentist.
What are mouth ulcers?
Mouth ulcers (oral ulcers) are open sores that can appear on the lips, cheeks, tongue, gums, and palate. They can be caused by minor irritation, infections, inflammation, immune-mediated conditions, and, less commonly, malignancy.
Quick triage: when to seek medical help
Seek medical attention if:
- the ulcer lasts longer than 2 to 3 weeks
- it is hard, raised, or has rolled edges
- it bleeds easily without obvious injury
- you have fever, weight loss, swollen lymph nodes, or severe fatigue
- ulcers keep recurring frequently, are unusually large, or are associated with other symptoms (eye inflammation, genital ulcers, joint pain, digestive symptoms)
1. Aphthous ulcers (canker sores)
Aphthous ulcers (canker sores) are the most common mouth ulcers. They are not contagious.
What they look like
- Color: white, yellow, or gray center with a bright red halo
- Shape: round or oval
- Edges: clearly defined, inflamed border
- Texture: soft base, very tender
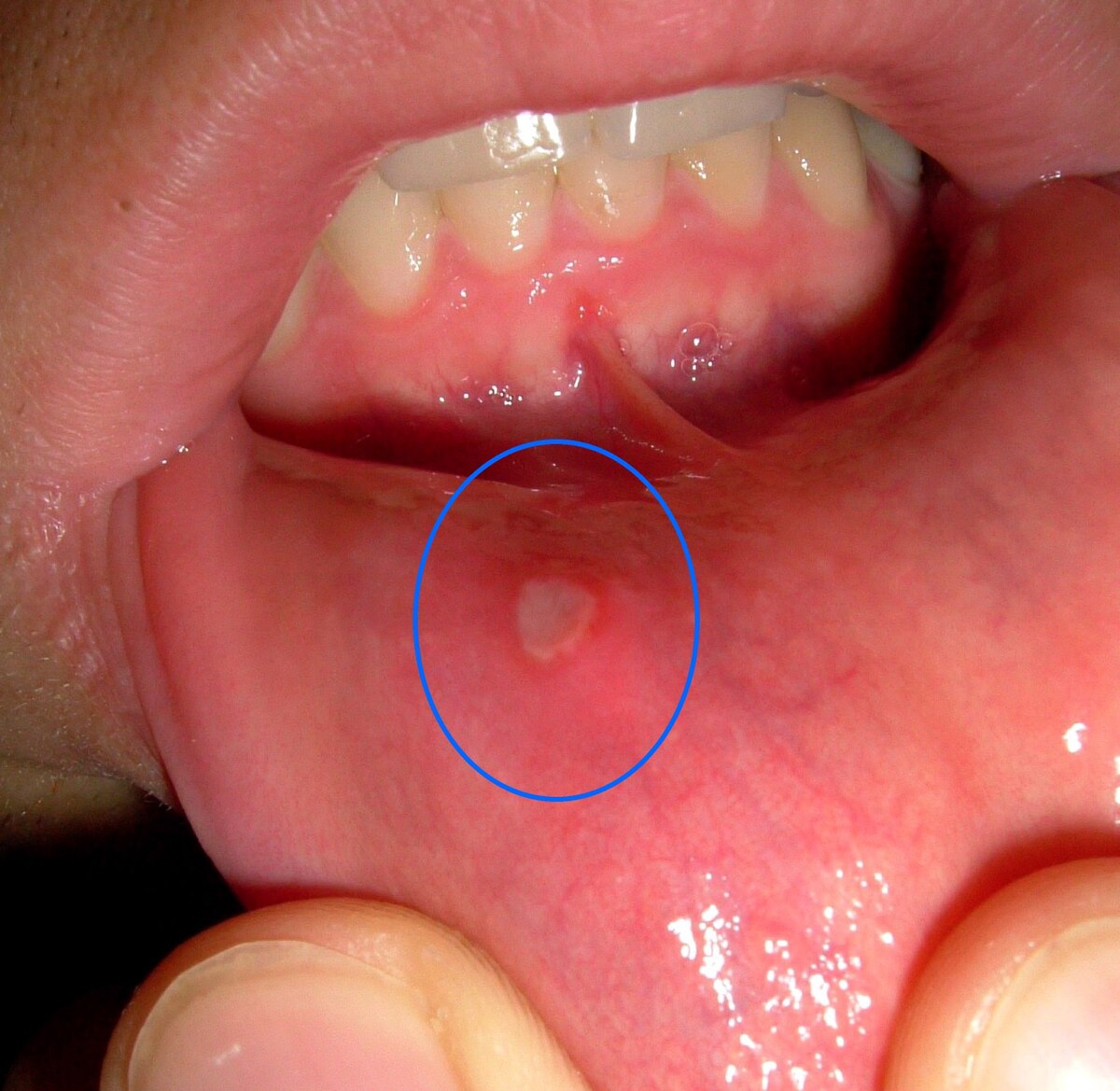
A classic aphthous ulcer (canker sore) with a pale center and red halo.

A second aphthous ulcer example.
Common locations
- inner cheeks
- inner lips
- tongue sides
- soft palate
How they feel
Often moderate to severe burning or stinging. They can look small and feel disproportionally painful.
Variants
- Minor aphthous ulcers: most common, smaller, heal without scarring (often 7 to 14 days)
- Major aphthous ulcers: larger, deeper, may scar (weeks to months)
- Herpetiform aphthous ulcers: clusters of tiny ulcers (not herpes)
Common triggers and associations
- immune system dysregulation
- stress, sleep disruption, or illness
- local trauma (biting, dental work)
- vitamin B12, iron, or folate deficiency
- gastrointestinal disease (for example, Crohn’s disease, celiac disease)
- hormonal changes
2. Traumatic mouth ulcers
Traumatic ulcers are caused by physical injury to oral tissue.
What they look like
- Color: white or yellow base with red inflamed margins
- Shape: irregular, often asymmetrical
- Texture: raw, shredded, or “scraped” surface

Traumatic ulcer example.

Another traumatic ulcer example, often from ongoing irritation (teeth, appliances).
Common locations
- along cheek bite lines
- tongue edges
- under dentures, braces, or sharp teeth/fillings
Healing time
Typically heals in about 5 to 10 days once the source of irritation is removed.
3. Herpetic ulcers (oral herpes)
Herpetic ulcers are caused by herpes simplex virus (HSV). They are contagious.
What they look like
- Color: red base with yellow-gray ulceration
- Shape: multiple small ulcers from ruptured blisters
- Texture: shallow and fragile

HSV lesions often start as blisters, then become small clustered ulcers.

Another oral herpes example.
Common locations
- hard palate
- gums
- lips (inner and outer)
Common associated symptoms
Burning or tingling, fever, fatigue, swollen lymph nodes, and widespread mouth soreness during outbreaks (especially primary infection).
4. Fungal mouth ulcers (oral candidiasis, thrush)
Oral candidiasis causes white plaques that can ulcerate, especially in people with altered oral microbiome or weakened immunity.
What it looks like
- Color: white or creamy plaques
- Shape: patchy, irregular areas
- Texture: soft, often scrapeable (may bleed underneath)

Thrush often appears as white plaques on the tongue or cheeks.

Another candidiasis example.
Common risk factors
- diabetes
- HIV/AIDS or other immunosuppression
- steroid inhaler use
- recent antibiotics
5. Oral lichen planus (ulcerative type)
Oral lichen planus is a chronic immune-mediated inflammatory condition.
What it looks like
- Color: white, lace-like patterns with red erosive ulcers
- Shape: linear or irregular
- Texture: rough, leathery, sometimes ulcerated

The classic “lacy” white pattern (reticular lichen planus).

Erosive or ulcerative lichen planus can look red and raw.
Why it matters
It can be long-term and needs monitoring. There is a small risk of malignant transformation, so persistent or changing lesions should be followed by a clinician.
6. Systemic disease-related ulcers
Recurrent, severe, or unusual mouth ulcers can be linked to systemic inflammatory or autoimmune diseases.
What they can look like
- Color: yellow-gray with intense surrounding redness
- Shape: large, deep, irregular
- Texture: crater-like or necrotic

Larger, deeper ulcers can be seen with some systemic inflammatory or autoimmune conditions.
Associated conditions (examples)
- Behçet disease
- lupus
- Crohn’s disease
- celiac disease
Extra red flags
- genital ulcers
- eye inflammation
- joint pain
- chronic digestive symptoms
7. Oral cancer (malignant ulcers)
Oral cancer can present as a persistent non-healing sore. Many early lesions are painless.
What it can look and feel like
- Color: red, white, or mixed red/white patches
- Shape: irregular with raised or rolled edges
- Texture: firm, indurated, may bleed easily

A non-healing sore with irregular borders should be evaluated promptly.

Another suspicious lesion example (location and appearance vary).
Highest-risk warning sign
If an ulcer lasts longer than 3 weeks, get it evaluated.
Mouth ulcer comparison chart (quick summary)
| Type | Color | Shape | Texture | Pain | Common cause |
|---|---|---|---|---|---|
| Aphthous (canker sore) | White/yellow center + red halo | Round/oval | Soft, tender | High | Immune + triggers |
| Traumatic | White/yellow base + red margins | Irregular | Raw | Variable | Injury/irritation |
| Herpetic (HSV) | Red base + yellow-gray ulcers | Clustered | Fragile | High | Virus |
| Fungal (thrush) | White plaques | Patchy | Scrapeable | Low to moderate | Candida |
| Lichen planus | White lacy + red erosions | Linear/irregular | Rough | Variable | Immune-mediated |
| Oral cancer | Red/white/mixed | Irregular | Firm | Low early | Malignancy |